Clostridium Perfringens
New ways to type strains of a deadly bacteria
 It has killed minks on a ranch in Montana, sheep in Australia, hundreds
of pigs and cattle across the U.S. and even a rare shoebill stork
at the San Diego Zoo. Exhibiting frighteningly violent and rapidly
progressing symptoms, Clostridium perfringens-induced intestinal
diseases have confounded livestock producers and veterinarians around
the world, along with medical doctors who at times have been stunned
to diagnose in humans what is more commonly considered an animal disease.
It has killed minks on a ranch in Montana, sheep in Australia, hundreds
of pigs and cattle across the U.S. and even a rare shoebill stork
at the San Diego Zoo. Exhibiting frighteningly violent and rapidly
progressing symptoms, Clostridium perfringens-induced intestinal
diseases have confounded livestock producers and veterinarians around
the world, along with medical doctors who at times have been stunned
to diagnose in humans what is more commonly considered an animal disease.
"The organism is so promiscuous in terms of its hosts that it’s
found wherever there are domestic animals," says Glenn Songer,
a veterinary scientist in the College of Agriculture at The University
of Arizona. "It makes a lot of toxins, and it’s almost always
lethal."
Many years ago scientists developed a scheme where they divided it
into five types based on production of four toxins. These four main
toxins--known as alpha, beta, epsilon and iota toxins--combined with
many other toxic substances created by the bacteria, produce nearly
25 different diseases.
Diagnosing a clostridial disease requires isolating the pathogen
and determining which toxins are involved. The three traditional means
have included
- growing the organism in liquid culture, getting rid of the bacteria
and looking for the toxins
- searching for toxins in the gut of an animal already dead from
the disease
- injecting the toxins into mice or guinea pigs and neutralizing
them with specific antibodies to see whether the toxic effect is
from that particular strain.
All of these methods have drawbacks, including the tendency to yield
false negatives by not being sensitive enough; false positives from
a lack of specificity; and a humanitarian concern with the guinea
pig and mouse assays. (They are no longer commonly used.)
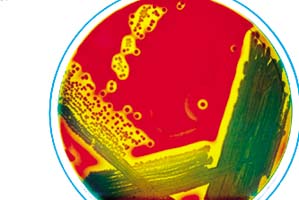
Songer has been working since 1990 with graduate student Ralph Meer,
now a UA nutritional scientist, and with Dawn Bueschel, a research
technician in the Department of Veterinary Science and Microbiology,
and graduate students to find a practical way to assay isolates of
the disease. They have developed what is called a multiplex polymerase
chain reaction (PCR) assay that allows simultaneous detection of the
four major toxin genes plus the gene for enterotoxin, for C. perfringens
in one test.
This represents a major breakthrough, since individual tests were
previously needed for each toxin. It also eliminates the "silent
gene" problem inherent in the other assay techniques, where certain
toxin genes went undetected. Because vaccines are only effective if
they target the exact toxin responsible for the illness in an individual
animal, this method will help speed diagnosis of C. perfringens
in disease outbreaks and assist the development of specific vaccines.
"We hypothesized that if the toxin is being produced, then the
gene has to be there," Songer says. "We thought maybe we
could replace toxin detection with detecting the gene for the
toxin. We developed a method based on polymerase chain reaction, where
a small number of DNA sequences are amplified. We determined the sequence
of the gene to make the primers and then developed the assays."
Songer and Meer took field isolates from animal, human and feed sources
and compared the genotypes they had found with the phenotype, or actual
physical attributes of the bacterial toxin production already established
through traditional assays. They obtained 100 percent agreement, first
using an assay in which they ran separate reactions for each of the
four major toxin genes. Then they adapted this to a multiplex test
to detect all four, plus the enterotoxin gene, simultaneously. The
test was up and running by 1994, and Songer says the UA lab has used
it to diagnose thousands of C.perfringens-related illnesses
at the request of community and scientific professionals.
"We get five to ten calls a week from people who want information,"
he says. "We’ve typed 3,000 isolates on request, from all
across the North America." The lab has served practicing veterinarians,
livestock producers, and professionals from biologics companies. The
tests usually focus on clostridial enteritis diseases in traditional
food animals: dairy and beef cattle, sheep, goats, pigs; plus some
cases with ostriches, llamas, alpacas, mink and horses.
When a very valuable thoroughbred foal died in California, Songer
and his team worked with diagnosticians from UC Davis to determine
the cause. "We were able to pin this down as a perfringens-related
death," he says. "We’ve also had extensive contacts
with the San Diego Zoo’s Center for Reproduction of Endangered
Species (CRES). The center breeds endangered animals in captivity
and then releases them into the wild. Songer’s team has assisted
them in preventing and diagnosing enteric diseases.
Although state veterinary diagnostic laboratories in Washington,
Texas, Kentucky, Alabama, Indiana and other states are using the test,
Songer says many labs still send their isolates to the UA. In some
cases biologics companies and livestock producers have been able to
work together to take isolates from the ranch animals and have the
company make a vaccine. "The idea is that if the organism is
in their own herd, producers can use that specific one to target the
disease with a vaccine," Songer says.
Through the UA Department of Veterinary Science’s web site,
Songer says he has gotten emails and inquiries from all over the world,
including South Africa, New Zealand, Norway, Canada and Japan. The
web site describes the multiplex PCR assay and gives instructions
on how to send in samples for C. perfringens genotyping. For
more information, view the web site at microvet.arizona.edu. Using
the navigation bar on the left side, click on "Research."
A Potentially Lethal Pathogen
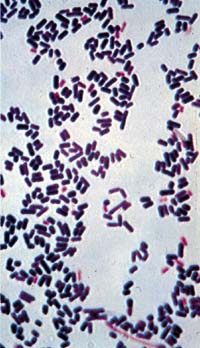
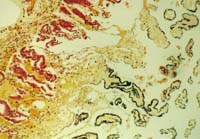
Once an animal contracts a disease caused by Clostridium perfringens
it’s often too late to do anything about it, according to Glenn
Songer, UA veterinary scientist. Death comes quickly and violently.
This type of bacteria, occurring in five different strains identified
by toxin type, produces a host of toxic proteins; nearly twenty have
been described scientifically and there may be more. These toxins
can act rapidly in the body, causing severe diarrhea, dysentery, gangrene,
muscle infections and various other forms of enteric (gut) disease.
The symptoms vary in intensity and variety depending on the individual
toxin and its host.
C. perfringens can cause disease in most domestic animals
and some wildlife, including horses, poultry, sheep, birds, rabbits,
goats, hogs, cattle, mink, ostrich, emu, dogs, cats, and others. Humans
have also become infected, although cases of enteritis have been localized,
most notably in the highlands of Papua New Guinea where it occurs
as a severe, usually fatal form of food poisoning that kills the small
intestine.
In spite of its potential danger as an infectious agent, the avirulent
forms of bacillus are commonly found in the intestinal tracts of warm-blooded
animals, and it also inhabits terrestrial, marine and aquatic environments.
The trouble starts when the balance of bacteria in the gut is disrupted,
giving C. perfringens a chance to proliferate unchecked. It
may contaminate soil, animal feed and litter, or be transmitted directly
from infected to healthy animals.
C. perfringens related livestock infections have been reported
in every state in the nation and in most parts of the world. Although
surgery can save human victims, it is often not feasible to perform
it on domestic animals. The most practical way to handle perfringens-related
illnesses in animals is to prevent them in the first place.
Article Written by Susan McGinley, ECAT, College
of Agriculture
This is part of the 1998 Arizona Experiment Station Research Report
This document is located at http://ag.arizona.edu/pubs/general/resrpt1998/clostridium.html
Return to index for 1998 report
Researcher:
Glenn Songer, Department of Veterinary Science
and MicroBiology
Phone: (520) 621-2962
gsonger@u.arizona.edu
|